I purchased a new smartphone.
Now, that may not sound like a bold leadership move, but hear me out. I had lived comfortably inside the Apple ecosystem for years. Decades, really. Back when the device was still mostly an iPod with aspirations. I stayed loyal through every upgrade, every new cable, every software update that required a quick “fingers crossed” before installing.
But over time, something strange kept happening.
The phone part of my phone stopped working.
Not once. Not twice. Three times.
Everything else worked beautifully. Camera? Great. Apps? Smooth. Storage? Well… actually, no.
Because along the way I also ran into another issue: I hit the dreaded storage ceiling. I offloaded photos. Deleted apps. Moved files. Cleaned out messages. Did all the digital housekeeping you’re told to do. And still, I couldn’t complete updates. My device simply didn’t have enough room to function properly anymore.
Which meant no updates. Which meant increasing glitches. Which meant growing frustration.
So let’s recap: a phone that struggled to make calls and couldn’t update itself. That’s less “smartphone” and more “expensive paperweight with a nice camera.”
And since I actually use my phone to speak with clients, record videos, and run meetings, this wasn’t a minor inconvenience. It was like owning a car with heated seats, satellite radio, and perfect leather interior…that wouldn’t start.
So I made a New Year’s resolution: be the disruptor.
I switched to a device from Google that integrates seamlessly with the tools I already use all day long. My photos sync instantly with my workspace. Files move effortlessly from phone to desktop. Content appears exactly where I need it when I’m building presentations or posting on LinkedIn. No workarounds. No digital gymnastics. No sending things to myself three times just to get them where they belong.
And, a small but important detail, the phone actually works as a phone.
The battery lasts. The storage expands in ways that actually support my workflow. And I’m not playing Tetris with files just to keep the device operational.
But the real surprise wasn’t the technology.
It was the reaction from everyone else.
Within hours, people noticed my text bubbles had changed color. Questions poured in:
“Why are your texts green?” “Did you get a new phone?” “Are you out of the country?” “Is everything okay?”
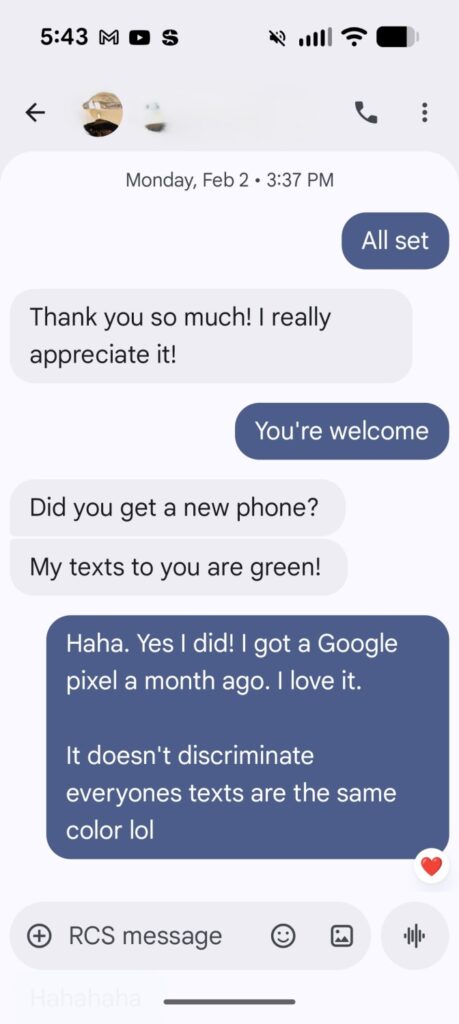
Apparently, changing a phone brand triggers the same level of concern as announcing you’ve moved to a remote island.
But here’s the part that made me laugh.
The emojis.
Now, I did not spend over $1,000 on a phone for emojis. Let’s be clear. But I will say this: they are delightful.
They move. They react. They animate. The eye-roll emoji doesn’t just sit there judging you, it actually rolls its eyes. And recently I discovered that if you type “boooooo,” your phone throws rotten tomatoes across the screen that splatter everywhere.
I laughed out loud. Alone. At my phone!
Which, honestly, felt like a small win for my daily stress level.
But beneath the humor, this whole experience got me thinking about something much bigger, something I see constantly inside medical and dental practices.
We assume there is a “right” way to do things.
Not the best way. Not the most effective way. Just the most common way.
And once something becomes common, it quietly becomes unquestioned.
Phones are a perfect metaphor for this. People stick with what everyone else uses because it feels safe. Familiar. Supported. Normal. Switching feels disruptive, even if the current system isn’t serving them anymore.
Sound familiar?
Because this happens in healthcare operations every single day.
I walk into practices that are using workflows no one truly understands anymore. Systems layered on top of systems. Policies no one remembers creating. Processes that frustrate staff, confuse patients, and slow down providers, yet remain untouched because “that’s how we’ve always done it.”
Let me give you a few examples I see regularly.
Some practices still dictate notes and use transcriptionists. That might sound outdated to one group and incredibly efficient to another. For some providers, dictation keeps them present with patients and reduces after-hours charting. For others, ambient scribe technology works better. Neither approach is universally correct. The right answer depends on workflow, specialty, staffing, and preferences.
Some practices build their own tech stacks rather than relying on a single EHR. They combine scheduling software, communication tools, intake platforms, and billing systems into a custom ecosystem. That sounds chaotic on paper, yet for certain offices it creates flexibility and efficiency that one monolithic system never could.
Some practices leave insurance entirely and move to cash-pay models. That decision can feel terrifying. It requires communication, planning, and a strong understanding of patient demographics. But for some providers, it restores autonomy, reduces administrative burden, and improves the patient experience dramatically.
These choices all share one thing in common: they break from the default.
And breaking from the default always creates friction.
When I switched phones, people didn’t just notice, they questioned it. Not because my choice affected them, but because it challenged the assumption that there was only one sensible option.
The same thing happens when a practice changes a long-standing workflow. Staff worry. Colleagues question it. Vendors sometimes resist it. Even patients may need reassurance.
Change feels uncomfortable because it disrupts expectations.
But comfort and effectiveness are not the same thing.
In fact, some of the questions I ask practices multiple times a day are deceptively simple:
What are you doing? Why do you do it that way? Does it work?
The answers are often revealing.
Sometimes there’s a thoughtful rationale behind a process. Sometimes there’s a regulatory reason. Sometimes there’s a clinical preference. Those are all valid.
But other times, the answer is:
“I don’t know.” “We’ve always done it that way.” “It kind of works… I guess.”
Those responses are opportunities.
Because if something doesn’t truly work; if it slows your team, frustrates your patients, or drains your energy; then the real question becomes:
Why are you still doing it?
Healthcare is full of smart, compassionate professionals who entered this field to help people. Yet many spend their days navigating systems that make their work harder than it needs to be. They stay inside those systems because changing them feels risky, time-consuming, or socially uncomfortable.
No one wants to be the green bubble in the group chat.
But sometimes the green bubble is exactly what you need.
When I switched phones, I didn’t do it to be different. I did it because my workflow needed something else. What I was using was no longer serving me. And once I made the change, the benefits were immediate. Communication improved. Integration improved. My daily friction dropped. It was a lightbulb moment!
It removes unnecessary effort.
It aligns tools with reality.
It lets people work the way they actually function, not the way someone assumed they would years ago.
Imagine applying that mindset inside a practice.
What if intake forms matched how patients actually complete information today? What if phone systems reflected how patients prefer to communicate? What if staff workflows were designed around reducing duplicative work instead of preserving tradition? What if leadership regularly asked whether each process still served its purpose?
Those changes don’t always require massive investments. Often they begin with curiosity.
Curiosity leads to evaluation. Evaluation leads to small adjustments. Small adjustments lead to meaningful improvement.
And yes, sometimes those adjustments will make you look different from your colleagues.
You may choose a different scheduling model. A different documentation process. A different patient communication approach. A different staffing structure.
Some people will question it. Some will watch skeptically. Some may even assume you’re creating problems for yourself.
But if the change improves your team’s experience, your patient outcomes, and your own sustainability as a leader, then the discomfort is temporary and the benefit is lasting.
The healthcare industry talks constantly about innovation. New technologies, new models of care, new reimbursement structures. Yet true innovation often starts with something much simpler: permission to rethink what feels normal.
My animated emojis aren’t revolutionary. The tomato-throwing animation will not transform healthcare delivery. But the decision behind that phone switch reflects something important.
Not everything is one-size-fits-all.
Not every popular solution is the right solution.
And sometimes the best improvement you can make is simply choosing what works for you.
So here’s my question for you:
What are you doing in your practice that is outside the norm…and working beautifully?
Maybe you redesigned your schedule and cut patient wait times in half. Maybe you implemented team huddles that transformed communication. Maybe you simplified documentation in a way that gave providers their evenings back. Maybe you built a tech ecosystem that fits your workflow instead of forcing your workflow to fit the software.
Those decisions matter.
Every time a practice thoughtfully challenges the default, it moves closer to something better, for patients, for staff, and for the clinicians who carry the responsibility of care every day.
Change isn’t easy. It can create friction. It can make you feel like the outsider for a while.
But if it leads to a more functional, compassionate, sustainable practice, it’s worth it.
Even if it turns your text bubble green.
Even if your colleagues raise their eyebrows.
Even if your phone occasionally throws digital tomatoes across the screen.
Sometimes disruption isn’t about being different for the sake of it.
Sometimes it’s just about finally choosing what works.