Most medical practices don’t fail because of a lack of clinical skill, technology, or effort. They struggle because of something much harder to spot, and much harder to talk about.
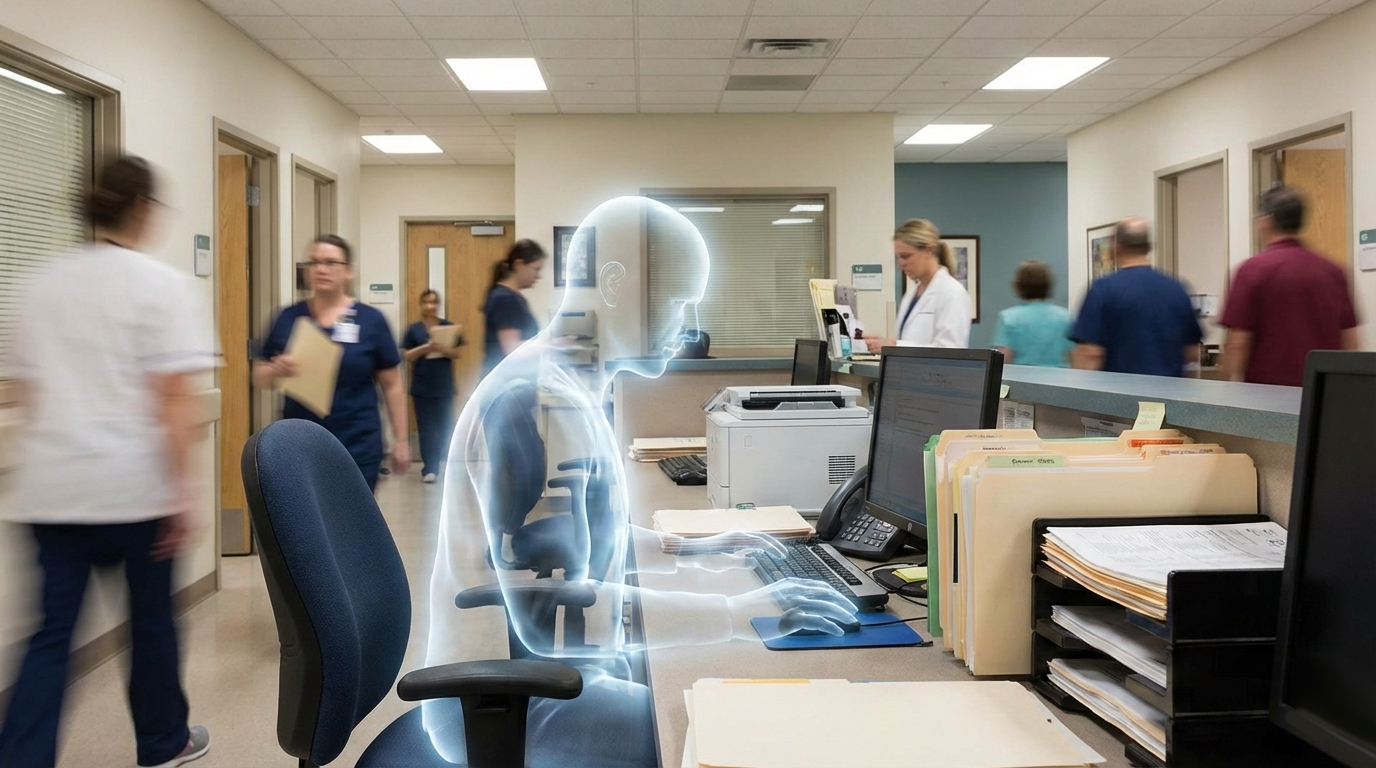
I call it “ghost mode”.
Ghost mode doesn’t mean your EHR is down. It doesn’t mean the phones aren’t ringing or that patients stopped showing up. In fact, ghost mode often exists in practices that appear productive, busy, and “fine” on the surface.
Ghost mode is more subtle. And over time, far more damaging.
It shows up as:
The practice keeps moving. Patients are seen. Encounter notes are signed/locked. Metrics are tracked. But morale flattens. Communication thins. And people slowly disengage…without anyone quite knowing when it started.
If this sounds uncomfortably familiar, you’re not alone. I see this every week in medical and dental practices of all sizes. Let’s talk about what ghost mode really looks like, why it happens, and, most importantly, how to come out of it.
Ghost mode isn’t laziness. It isn’t indifference. And it definitely isn’t incompetence. Ghost mode is what happens when good people get stretched too thin for too long.
It’s leadership on autopilot. It’s communication reduced to task lists. It’s decisions made quickly, but not always clearly.
In healthcare operations, ghost mode often shows up when:
No one intends for this to happen. In fact, most leaders in ghost mode care deeply. They’re just exhausted, busy, or unsure where to start fixing things. And because healthcare rewards productivity, ghost mode can look like success, for a while.
Ghost mode doesn’t always announce itself loudly. It whispers. Here are some of the most common ways it appears.
1. Physically Present, Mentally Checked Out Leadership
Leaders show up. They’re in the building. They answer emails. They attend meetings. But their attention is split, between patient care, compliance issues, staffing shortages, payer problems, and everything else competing for their bandwidth.
Staff can feel this immediately. When leadership presence is inconsistent or distracted, teams stop engaging fully. Questions go unasked. Concerns stay unspoken. People do the bare minimum to avoid rocking the boat.
2.Decision Paralysis – or Decision Confusion
In ghost mode practices, teams often don’t know:
Sometimes decisions are made quickly, without explanation. Other times, decisions are avoided altogether. Both create the same result: uncertainty, which quietly drains confidence and accountability.
3.Silence That’s Mistaken for Agreement
This one is especially dangerous. Meetings are quiet. No one pushes back. No one asks questions. On the surface, it looks like alignment. In reality, it’s often disengagement. When staff stop offering feedback, it’s rarely because everything is perfect. More often, it’s because they’ve learned their input doesn’t matter…or feels unsafe.
4.Productivity Without Engagement
Ghost mode practices often hit their numbers:
But behind the scenes:
Efficiency without engagement is short-term success at best.
Healthcare is uniquely positioned to create ghost mode, even in strong practices.
Constant Pressure
Between staffing shortages, reimbursement challenges, regulatory changes, and patient expectations, most leaders are operating under near-constant pressure.
When survival mode kicks in, reflection drops off.
Over-Reliance on “We’ve Always Done It This Way”
Old workflows linger long after they’ve stopped serving the practice. Leaders know something isn’t working, but changing it feels overwhelming. So the practice keeps moving forward…without really moving forward.

When nothing changes…nothing changes!
Unhealthy Ego (Both Kinds)
This is important, and often misunderstood.
Both create confusion. Both weaken trust. Strong leadership isn’t about control or avoidance,it’s about clarity and presence.
If you’re reading this and feeling slightly uncomfortable, that’s okay. Awareness is the goal, not blame.
Ask yourself:
If these questions feel hard to answer, that’s not a failure. It’s information. An opportunity for improvement.
Ghost mode doesn’t just affect morale. It impacts nearly every part of practice operations.
Staff Retention
People don’t usually leave because of workload alone. They leave because they feel unseen, unheard, or unsupported.
Patient Experience
Disconnected teams struggle to deliver consistent, compassionate care. Patients can feel it, even if they can’t name it.
Leadership Burnout
Leaders in ghost mode often feel isolated. They carry everything themselves, unsure how to re-engage their teams without creating more work.
Financial Performance
Turnover, inefficiency, rework, and disengagement all have real financial consequences, often hidden until they become unavoidable.
The good news? You don’t need a full restructure, a retreat, or a new EHR to reset. Small, intentional shifts make a big difference.
1.Increase Visibility (Not Surveillance)
A daily or weekly walk-through. A short huddle. A simple “How’s today going?”
Presence builds trust faster than policies.
2.Name the Disconnect
One of the most powerful phrases a leader can say is:
“I think we’ve been a bit disconnected. Let’s reset.” You don’t lose authority by naming reality, you gain credibility.
3.Clarify Decision-Making
Be clear about:
Clarity reduces anxiety and empowers teams.
 4.Create Feedback Without Fear
4.Create Feedback Without Fear
Psychological safety isn’t a buzzword. It’s a prerequisite for efficiency. If people don’t feel safe speaking up, problems stay hidden until they become crises.
Presence isn’t soft. It’s not optional. And it’s not inefficient.
Presence:
In healthcare operations, presence is often the missing link between chaos and calm.
The start of a new year invites reflection, not resolutions, but recalibration.
Ask yourself:
You don’t need to fix everything at once. You just need to start paying attention.
Many practice leaders I work with know something feels off, but don’t have the time, space, or internal capacity to step back and assess it objectively.
That’s where fractional practice administration can be incredibly powerful.
Fractional support isn’t about replacing leadership, it’s about:
Sometimes what a practice needs most isn’t another system, it’s a steady, experienced partner to help reconnect the people, processes, and priorities already in place.
If you’re wondering whether your practice might be operating in ghost mode, and want a calm, practical way forward, I’m always happy to start with a conversation. Because presence and perspective changes everything. And calm is built with one intentional step at a time.
